For the past three or four weeks, spinning a breech baby has been our preoccupying obsession. Our baby has been breech for a while, but for half of our second and much of our third trimester, the message we got from all corners was, “Don’t worry; it’s highly likely she’ll flip.” So we trusted conventional wisdom and did nothing, until we got to nearly 36 weeks. That was when we realized we needed to start being proactive. Yesterday she finally flipped. It has been an incredibly intense journey getting here, and I just need to write about it, because it has become it’s own chapter in baby C’s birth story. So hang in there, this is going to be long, because it is both a re-telling of our story and a review of a number of medical techniques. It has precious little to do with knitting, except in the Psalm 139:13 sense. And who knows, maybe our experience will help someone going through the same thing.
Cyrilla was first noticed to be breech on ultrasound at 20 weeks. We thought nothing of it, because at that stage, babies move all over the place. At 28 weeks, we still thought nothing of it, because up to 25% of babies are breech at the beginning of the third trimester, and most of them turn on their own. Only 5% of babies are still breech at the beginning of the 9th month (35 weeks), and only 3% are still breech at term (37 weeks).
We listened to these statistics, and we felt justified in doing nothing. I became familiar with the feeling of her little head poking uncomfortably at the top of my belly, little wannabe xenomorph that she is. But by the time we got back from our holiday travels and got situated again, we were past 35 weeks, and starting to get nervous.
Why were we nervous? Because in the USA right now, standard practice is that breech = Cesarian section. This is because of a study done around the turn of the millenium that said that statistical outcomes are slightly better if you do a routine Cesarian for breech rather than trying labor. The study was overall pretty solid, but it was ended early and had some issues. But it was enough to turn the world of vaginal breech birth upside down. Doctors (at least in the US and Canada) stopped offering vaginal breech birth, and they stopped training their doctors on the complex maneuvers that make breech birth safer. Meanwhile, as this practice of routine Cesarian for breech was being implemented, the evidence was showing that while Cesarian breech slightly lowered the risk of neonatal mortality/morbidity (death/injury for babies), because of the inherent risks in Cesarian, maternal mortality went up.
Now, Canada took a really hard look at its policies and redid their own studies, so that as of 2010 they now offer and even encourage moms who are breech at term to try to birth vaginally. This is because, if you select out moms for certain criteria, it is just as safe to attempt a vaginal breech birth for a frank or complete breech baby as it is to attempt a vertex (head-down) delivery, and there are other significant benefits to vaginal birth. They also retrained doctors across Canada to be competent to perform breech deliveries. You can read all about their policy in this document, which is fascinating (at least if you’re dealing with the subject yourself), and you will probably find it easy to read if you get through this post.
But the US, as seems to be the case in most things birth-related, is behind the times. So we found ourselves at 36 weeks finally getting to know the awesome midwives at The Midwife Center, who operate under the auspices of the doctors at UPMC Mercy hospital. Neither of these places will even attempt a vaginal breech birth. As someone who is freakishly passionate about wanting a natural birth, we decided to start doing something about our situation.
Right away, I started a few things that anyone can and should do at home. I talked to my baby about turning every day, and Jared did too. Jared started talking to the bottom of my belly – If you don’t have a husband with a lovely resonant voice like mine does, you can play a recording of your own voice, or just hold any vibrating larynx-like object (like a sonic toothbrush) to the bottom. This did diddly squat for us, but I’ve heard it works for some people, and it was fun. I started working on my posture, as leaning back in what our childbirth instructor calls “TV-watching position” encourages baby to stay breech and/or posterior (back to your backbone, not ideal for labor). Sitting up straight, leaning slightly forward, is much better when pregnant. And of course, we prayed about it together at least tdaily. We asked lots of people to pray. And every time we tried one of the techniques listed below, we prayed. This tells you a little bit about how far in the forefront of our brain this whole issue became. For most people, the last few weeks of pregnancy seem to take forever because you’re just waiting for something to happen any time; for us, life slowed to a crawl starting at 35 weeks because we were working and hoping so hard for baby to turn.
Thing #1: The first thing we tried was Moxibustion. Moxibustion is an acupuncture technique in which, basically, a stick of mugwort incense is waved near a pressure point on each pinky toe, one at a time, for 15 minutes each. Yes, that’s it. This is actually a legit technique that’s been around for a while, long enough for a few studies to have been done on it. The idea is that the incense warming that pressure point stimulates the release of hormones that cause the baby to turn. Supposedly, this slightly increases the chances that your breech baby will turn, especially if you start at 34 weeks. (Of course, remember, about 70-80% of babies who are breech at 34 weeks will flip by themselves before they’re born.)
About this technique: you will have to lie down on your back for a little over half an hour for this procedure. The acupuncturist will light a stick of incense, which looks rather like a long cigar, and will wave it near each pinky toe – fifteen minutes on one side, then the other. It feels pleasantly warm and shouldn’t burn. There are other ways to do it that do burn, and still others that require you to go into the acupuncturist every day, but I don’t know that they’re any more effective. With this technique, I paid 65$ for one visit. There, the acupuncturist showed me how to do the technique and gave me a couple of sticks of incense. I then showed Jared how to do it, and we did it at home. You do it for five days on and two days off.
We did indeed do it for five days on, two days off, and one day on again, starting at 35 weeks, 6 days. After those eight days, baby still hadn’t flipped, and our house was starting to seriously smell like moxa (mugwort), which smells awkwardly like pot. I felt like I was breathing a lot of smoke to no purpose, the house smelled like we were potheads, and our moxa sticks were running out, so we gave up on moxibustion on the same time that we tried our second technique for baby turning.
Thing #2: The second thing we tried was External Cephalic Version, without medication. External Cephalic Version, or ECV, literally just means “turning the baby head-down from the outside.” You lie down and a doctor grabs the baby from the outside of your body and tries to get him or her to flip around, guided by ultrasound. We tried this at 36 weeks, 5 days.
About this technique: This technique happens in hospital. You will have to fast from the midnight before the procedure, because of the minute chance that it might break your waters or hurt baby in a way that requires a C-section. Because of this you will also have to have an IV heploc installed. Again, you are on your back. The procedure starts with ultrasound, double-checking that baby is still breech. You’ll then get smeared all over with gel, and the doctor will start grabbing at you. He starts by trying to get the baby’s butt up out of the bottom, narrower part of your uterus. If he can get that part up, there’s a good chance that he can get the baby to flip. Still, external version is only successful around 30-40% of the time, and even then, baby can flip back (though it’s highly unlikely in a first-time mom, since there’s not a lot of extra room in there). Safety-wise, a very small amount of the time this causes you to go into labor, or to need an emergency C-section, but no baby has died from this procedure (except twice in Zimbabwe with no ultrasound) since it became a commonly available practice. Doing an ECV without anesthesia of any kind is even less likely to cause these complications, because it’s painful (the doctor is pushing HARD), and your own pain level is going to prevent them from doing anything to push baby so hard that something undesirable happens. This is a good thing, as you probably don’t want to pump your body (and your baby) full of drugs if you can avoid it, and it’s a great opportunity to practice your breathing and pain coping techniques. Whether or not the procedure succeeds, they’ll keep you for about 30 minutes afterwards, attached to the fetal monitor to make sure baby tolerated being pushed around.
What I didn’t quite realize about this procedure going in is that it is a hospital procedure. You will have to change into a hospital gown and lie in a hospital bed attached to a fetal monitor both before and after. Because our doc was in surgery at the time of our appointment, and things in hospitals take forever anyway, we were in that room for 2 hours before they did the procedure. Now, the last time I was in a hospital I was 16 years old, and it was among the most disempowering experiences in my life, coming at the absolute lowest point in my life. That experience is largely why I dislike hospitals, though I didn’t really realize this until I spent those two hours trapped in a hospital bed, extremely hungry, replaying that old trauma in my head.
In the room with us for the version were the doctor, a nurse, and two residents observing the doctor, who is very experienced with this technique. The procedure was difficult, painful, and didn’t work after two tries. Plus the doctor discussing the procedure with the residents made me feel a bit like a science project. Baby’s butt was trapped in the bottom part of my uterus like it was a Chinese finger trap. Immediately after it didn’t work the second time, the doctor (bless him) wanted to have a conversation about scheduling a C-section before our due date. Already reliving old trauma and in pain, I was almost unable to speak words for myself, and it was all I could do to say we’d think about it and get him out of the room before I started crying. Bless the one nurse with terrible teeth who took care of us the whole time, and was the one person who squeezed my hand and said encouraging, sympathetic words both during and after, and got us out of there as quickly as possible. The best thing that came out of the experience was the realization that I needed to really pray and start dealing with my past trauma about hospitals, because it was all too likely that I was going to go through a C-section in one, and I didn’t want to be totally messed up emotionally and mentally if that’s what went down. I’m glad we had that advance hint that I needed to deal with that.
As it happened, after this procedure we had about enough time to go out to Chipotle for dinner before heading to our childbirth class. I was so discouraged, especially that week as we sat in class learning about natural birth, which I wanted so badly and was starting to realize I might not get. And my hand hurt like the dickens from the IV. When I am really sad about something, my inclination is to go be by myself and process my emotions and then talk about it, maybe, with like two people. Thankfully, Jared’s inclination was to go talk to anyone he thought could help – so he got into a conversation with our childbirth instructor. She is also a certified prenatal yoga instructor, and trained with the ladies behind Spinning Babies.
By the way, I have to plug our childbirth teacher, Deena, right now. She stayed behind us after class and showed us all this stuff that very night, no charge. She’s an educator, so she’s about sharing the research and the rationales, which thinky-thinky me really needs. Her studio is called Shining Light Prenatal Education, which is also a prenatal yoga studio. It’s in the Lawrenceville neighborhood of Pittsburgh, and I’d recommend her classes to anyone.
So that evening, we got introduced to Thing #3: At-home version exercises. Now, I had about thirty people recommend the spinning babies website to me, and I’d spent one anxious night reading it. The whole thing seemed very confusing and overwhelming, and the techniques didn’t make a lot of sense to me. I had tried a couple of inversions on my own, but it seemed kind of silly. So it was invaluable to me to have someone experienced show us exactly how to do the things, explain why they were important, and give us a little routine to do every morning and evening. The routine took about 5-10 minutes, required Jared’s help, and then I was to lie down either on my side with one knee bent or in the breech tilt for at least 20 minutes.

About these techniques: The exercise routine she gave us mostly involved “rebozo sifting” (me on hands and knees, with Jared lifting my belly in a wide scarf and jiggling it around until his arms got tired) and “inversions” (various things to get your butt higher than your shoulders). Both of these types of techniques try to wake baby up and “release the psoas,” which I don’t have enough anatomy to quite understand. But the basic rationale is that there’s a muscle called the psoas that is part of why baby’s butt gets stuck down south, and these techniques help get it unstuck. After it’s unstuck, many babies will flip themselves, and the lying down part after the exercises gives her a chance to do that. You can lie down on your side, with your bottom leg straight and your top leg bent and raised on pillows, or in the breech tilt position (lying flat on your back on a plank tilted about 20 degrees, with your head at the lower end. We rigged one up with a couch, an inverted coffee table, and a lot of pillows).
We started these exercises at 36 weeks, 5 days. We did our exercise routine, followed by a nice lie-down, with religious regularity twice daily for a good two weeks. We tried to do it a little bit after I’d eaten something, so baby was nice and awake and active to try to turn herself afterwards. (If baby isn’t moving while you do the exercises, it’s best to give up and try again later.) We used our Moby D for a rebozo, since the solid panel in the center is conveniently belly-shaped. We put a folded blanket on an area rug and called it a yoga mat. Towards the end of two weeks, I was starting to really feel like her bum was coming free sometimes, and we did more of the breech tilt. Our stubborn little girl seemed to enjoy the attention – she especially liked to kick around during the rebozo sifting – but despite our efforts, she still didn’t want to turn around on her own.

There are a couple other at-home techniques I should mention. The first is temperature: pairing a bag of frozen peas at the top of your belly with a heating pad at the bottom. Supposedly baby wants to get his head away from the nasty cold thing and toward the nice warm thing. Our baby certainly didn’t like having frozen peas on her head, but she tried to solve the problem by headbutting the bag off, then by retreating further down into my pelvis (bad). I loved the heating pad though; I often used it during my post-exercise lie-down to encourage the release of those mysterious southern muscles. It just felt nice; who cares if it did anything. The other is the flashlight trick. I originally misunderstood this: I thought you tried to get the baby to follow the flashlight down like a cat. But according to Deena, you’re trying to shine a light into baby’s eyes to startle her so she frees herself and turns around. We couldn’t get our girl to react to a flashlight at all.
Around the same time, we got a reference from the midwife center for a chiropractor who could do Thing #4: The Bagnell Chiropractic technique. This was pretty cool: for either Bagnell or its ancestor, the Webster technique, the basic idea is that the chiropractor gets you nice and aligned, then does some extra things to line up your pelvis. This helps release tension in your back and in the long ligaments that go up around the side of your uterus (perhaps also the psoas? I don’t really know). This helps your uterus relax as much as possible, giving baby as much room to flip as she can get.
About this technique: First off, I’d make sure to find a chiro who is experienced in this technique. You’ll go in for a long first assessment, then about three times a week you’ll go back and keep getting adjusted until baby flips. My chiro adjusted my neck every time, then my back, then spent a long time doing funny things with my legs and pelvis.
Chiropraxy is a mystery to me, but I love it. I carry a lot of tension in my neck and shoulders, and it feels lovely to hear that beautiful crack and release when my neck gets adjusted. I also love touchy chiros, none of this strap-you-into-a-machine-that-pulls-0n-your-neck stuff. My chiro had a way awesome bed with a springy bit that meant I could lay on my stomach with my belly supported but unpressured. I started chiro at 37 weeks, 3 days.
This technique is great for giving your baby the chance to turn, but again, it depends on baby to do it himself or herself. And our baby was just not interested. Which leads us to thing #5. Thing #5 is a long story in itself – the story of how our baby finally turned.
Through our childbirth instructor, we’d heard a little tale about a practice at another hospital with two doctors who were actually open to doing vaginal breech birth. I was so discouraged at this point, it was so late in the game, and I had already changed care providers twice during this pregnancy, so I was going to just let this one go. Also I have an unreasonable hatred of making phone calls. But Jared kept encouraging me to try things, so we made a deal: I would call the chiropractor, and he would call this doctor. I dutifully started chiro 3x a week, and Jared started a series of phone calls coordinating between Magee Women’s Hospital and the Midwife Center. Before I knew it, we had a consult set up with this breech-experienced doctor. (A tip from one of our midwives: if he looks “young and moisturized,” your doc probably doesn’t know how to do vag breech deliveries. To be both trained and experienced with breech, he has to be kinda old.)
We had a lovely conversation. He gave us the whole history (most of which I knew) of breech birth, the way they used to do things, and the study that changed everything. Cesarian is still not recommended for breech at this hospital and every other one in America, but because a few doctors here have experience, at Magee it’s an option for women who meet certain criteria – having a frank or complete breech, going into labor naturally, having the head tucked, that sort of thing. They also are much more okay on doing it for a woman with a “proven pelvis” – i.e. who have had at least one head-down vaginal birth, or a multiple birth where the second baby is breech. Obviously, I didn’t meet this requirement. But, as this doctor said (and good grief do I ever love him for it), they can’t strap me down and force me to let them cut my baby out. So, if I was willing to have my pelvis examined both manually and with a CT to make sure it was not unusually small, he’d poll the doctors and see who was willing to let me try. (Of note: in Canada, first-time moms who seem to have a normal pelvis based on just a manual exam, not even a pelvic CT, are considered good candidates for a breech attempt if they meet the other selection criteria. Meaning in Canada I would be recommended to try a vaginal breech delivery) He couldn’t guarantee that a willing doctor would be available when I went into labor, and out of those moms who do meet all their criteria, only about 50% succeed. For many reasons, most of the rest have c-sections, and of course there is the rare tragedy where baby’s head gets trapped in the cervix, resulting in nasty nasty emergency surgery for mom and probable permanent brain damage or death for baby. And he confessed frankly that most doctors would think we are crazy for even having this conversation. But good golly, I would take some chance over no chance. And it felt so, so good to have my preferences admitted as possible, to have my wishes respected, and to have a choice again.
But it was in the midst of this conversation that Thing #5 came up. Another option this doctor offered was to attempt a version once I’m in labor, with an epidural. Now, I’ve heard a good bit about epidurals, and we learned in our childbirth class how they are administered. Frankly, I don’t fancy the idea of having to get one inserted in the middle of labor. So I asked, would there be any advantage in trying this before I went into labor? He said that was a great idea; how about tomorrow?
So that’s how we found ourselves back in the hospital yesterday morning, trying Thing #5, External Cephalic Version with Epidural (and muscle relaxant). Talk about a hospital procedure! It’s just what it sounds like – they check to make sure you’re still breech, give you IV fluids and an epidural, then go through the same procedure as described above. Only this time, they are not limited by your pain tolerance (though it’s still uncomfortable, and you still have to breathe carefully and deeply through baby getting shoved up into your lungs). Because they’ve done more to you, and you have to recover from an epidural (not my favorite thing), you have to stay at least a couple hours for monitoring afterwards instead of just 30 minutes. The only other difference in this case for me was that I was told not to eat or drink since midnight beforehand – at least partly so my bladder would be empty. This makes a lot of sense, because they are trying to get baby’s head to go where your bladder lives.
We had a much better attitude going into this procedure, since we largely knew what to expect, and I had no expectation that it would work. (According to the doc, an epidural only adds 10-15% to the chance of success of an ECV.) I had spent the last two weeks studiously and prayerfully working through my hospital issues. I had largely reconciled myself with the possibility of a Cesarian, and I was tremendously encouraged by the knowledge that even if this failed, I still had a chance (albeit a small one) for a vaginal breech birth. The nurses were all sweet and treated me like a person, the doctors were personable and respectful, and I’d gotten used to the brusque self-importance of the average resident. It was also very early, so I wasn’t as starving. The epidural went in smoothly, with much less pain than an IV, and rather than think of all the risks and dangers of epidurals, I enjoyed the novelty of my tingly legs. The first dose of epidural anesthetic didn’t reach quite high enough, so the anesthesia resident gave me a higher dose, which knocked out my legs entirely and numbed me to the top of my belly.
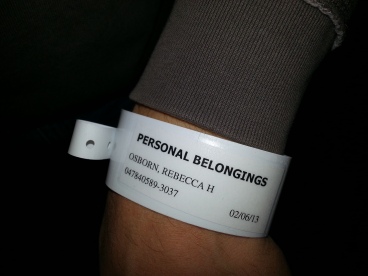
(above: life as a regular hospital patient. Yuck. below: Jared tagged as my “personal belongings.” That bracelet we are keeping!)
The doctor of the previous day’s consultation, whom I’ll call Dr. P (his name doesn’t start with P), attempted the version together with Dr. B. (I will tell you they were both very polish names. This whole vaginal breech thing seems a bit on the down-low, so I don’t want to advertise this lovely doctor all over the internets. But if you’re in the Pittsburgh area and in need, let me know and I’ll be the little bird to pass his info to you.) The previous time, there were only two hands on my belly, but now there were four, working together. Because they had to communicate, I could hear exactly what their strategy was: move the baby until she resisted, then wait for a minute until she relaxed. When they waited for her to relax, I would take that as a cue to relax those parts of my body that I could feel, which I knew would relax my uterus too.
During that first attempt, they got her butt out of my pelvis pretty quickly. (For that, I completely credit the daily exercises and regular chiropraxy.) However, when they got her halfway out, things went a bit “pear shaped” as the brits say. My chest suddenly felt heavy, and it became hard to breathe, which I informed the doctors of immediately, and they stopped. Soon I felt dizzy and nauseous, and was seeing the room fill with doctors and nurses through a golden haze. I heard them mention my blood pressure, which sounded like a very low number compared with what they usually tell me. I knew it was bad, but after a youth of watching medical shows, I didn’t flip out; I just concentrated on breathing into the oxygen mask. Jared said that they took all the equipment out of the room and hung my IV on a pole, and it looked for a moment like they were going to wheel me out of there. But my BP started coming back up, and the whole time they kept telling me baby was okay, and I heard baby’s heart rate on a the monitor solid as a rock. Once they stabilized me, then I started processing what had just happened, and had a good cry. They fixed up a bunch of things, let me breathe as much oxygen as I wanted, and said they’d give me a half hour to recover before trying again.
They don’t know exactly how this “hypotensive episode” happened; it was probably a combination of that high second dose of epidural and being flat on my back during the version. I expect more of the former, though the episode itself was probably brought on by the latter.
That was pretty ruddy scary. It’s such an example of the worst thing about hospitals – you go in completely healthy and not-sick, then twenty interventions later you have unstable vitals and feel like you got run over by a truck. Hospitals do lots of amazing things, and I knew I was in there to attempt to save a vaginal birth, so it was worth it. But the nastiness is just part of the package.
I felt pretty awful, as I had started to get the shakes from the epidural, and had a headache and nausea. They also had me propped in an awkward sort-of-side-lying position in which I couldn’t relax very well. I couldn’t believe they had talked about trying again in half an hour, and I had started talking to Jared about telling them we’d rather not when they bustled back in. Drs. P and B were discussing their strategy animatedly, and they sounded determined and positive, so I decided to let them have a go. This time I took lots of deep breaths, with oxygen, and firmly clamped Jared’s hand the whole time. I didn’t quite believe them, when after a bunch of maneuvers, they said “baby’s vertex!” held here there for a few minutes to make sure she would stay, and declared that we should give the baby a Polish name.
I had spent the last three weeks imagining what I would feel like if I felt baby flip. I thought I would be overjoyed, tearful, relieved, etc. In the moment, I was grateful, but at that point I was so used to having my hopes dashed that I was very skeptical. Also, I felt like complete crap. I spent the next hour with the shakes and nausea as the epidural wore off (this would not be great for breastfeeding, folks!), and they kept us another hour after that for more observation, and it took another hour to get all the tubes and monitors off and out of me and get us out the door. I suppose after all that, they wanted to make sure I was extremely stable, and that I could keep food down and walk.
So instead of a sudden moment of joy, we had an entire afternoon and evening of slowly melting incredulity. Our baby is head-down! We can have a natural birth at the midwife center! … No, really! Seriously? Yes, seriously! During the interim between the hospital and our last childbirth class, we took a nap, and joyfully informed everyone who had been praying for us. And I’ve been getting used to a new set of sensations as baby explores her new orientation, kicking and punching and headbutting and butt-pushing in new places. After confirmation from the midwives at our appointment this morning that she’s still head-down, I feel downright giddy.

In review, if this whole breech situation were to happen again, I would do a few things differently.
First, if I’m ever pregnant again at all, I would spend the whole pregnancy doing more walking, working on posture, and getting chiropraxy. I was limited in my amount of walking because of my issues with pubic symphisitis, but I could have done much more than I have done if I had made the time. As to posture, I thought I was incurably lazy, but the symphisitis forced me to change a lot of things because of pain, so I know I can do better. And chiropraxy I still tend to think of as an “extra,” a sort of fru-fru thing, but it’s actually great to do all during pregnancy, or at least during the second half. It releases tension, helps you be able to have good posture, and maximizes your pelvic area for delivery. And it’s not “extra.” I gather that from the fact that my Medicaid health plan pays for unlimited trips to the chiropractor when pregnant, with no referral. PA healthcare is awesome, but not to the point of paying for fluffy things. This is good, important stuff.
Second, I would ask around in advance to find doctors who are open to vaginal breech birth. Even if you find one, they might not do first-timers, but it’s good to have that last-ditch small-chance possibility in your pocket. We got tremendously lucky even finding one who would talk to us at 38 weeks 4 days.
Third, I would start doing exercises and extra chiropraxy stuff (Bagnell or Webster or whatever, but 3x-week) starting at 34 weeks, if baby was still breech. I might also do Moxibustion again, starting early, since the exercises include that nice lie-down time anyway. That stage of pregnancy is optimal flipping time, before things get really urgent and you get stressed out because you’re baby’s due what seems like tomorrow. If your baby is going to flip on its own, which is at least fairly likely at that point, you’re just helping him or her. And I DO credit the two weeks of exercises and Bagnell that we did squeeze in for how easily the doctors got her butt free at the second version attempt.
Finally, if baby is still in that stubborn 3% who get to term without flipping, I’d go for the version. I might still try the no-pain-meds method first, and failing that, try the epidural method a week later (it takes a few days to recover from your belly feeling kinda bruised). It’s a big intervention; it’s kinda scary; but to me, vaginal birth is worth it.
P.S. oh, and I would totally get a maternity chestburster shirt. Don’t google those three words together unless you loved the Alien movies and have a morbid sense of humor.
In closing, I have to praise God for making all this possible. For Deena, our childbirth instructor, who gave of her time, and gave us the crucial link to the doctor who could flip her. For Dr. P, for having that “crazy” conversation, giving us our sense of respect and agency back, and for both him and Dr. B for that heroic second effort that got her head-down. (We would so give her a Polish name if we weren’t so attached to the one we’ve picked for her!) And above all, for my husband. Jared was the one who encouraged me to try every avenue, when I was so busy processing my discouragement that I wanted to give up. Who listened to me when I was sad, and didn’t push too hard. Who helps me remember to take vitamins, and did those exercises with me every morning and evening. And who is himself so committed to natural birth, and has become sufficiently educated about both it and about my situation that he was able to make that phone call to Magee to set up the consult with Dr. P. There’s “I couldn’t have done this without you,” and then there’s “You made this possible. This literally would not have happened without you.” At we reach the end of this saga, I feel incredibly prepared: to work as a team with my husband, to cope with being in a hospital if we end up in that 15% of Midwife Center patients who have to be transferred, and to be positive if if I end up in the 1/2 of those who end up with a c-section. And if the highly unlikely happens and she flips back, we have a backup plan, or we might just schedule a C-section and be fine with it. Natural birth (and failing that, vaginal birth) is hugely important to us, but I am grateful, in the end, to live in a country where I’m nearly guaranteed a healthy baby at the end of it.
We are the Osborns. We are 39 weeks pregnant tomorrow. Bring it on.

Thanks for your article, which I forwarded to my daughter-in-law in the Phoenix area. She teaches the Bradley childbirth method. I had four children using the Bradley method (more or less), so no drugs. The most important aspect of the Bradley approach to childbirth, in my opinion, is the arming of oneself with knowledge of this most amazing and miraculous process by which a new human being enters the world.
LikeLike
Rebecca, thank you for sharing all that you and Jared have gone through. I’m so happy that the baby has turned! The Lord uses our experiences to help others in the same situation, and I’m sure yours will help more new mothers. He doesn’t waste a thing! You and Jared are going to be such wonderful parents. Thank you for letting us share this journey with you.
LikeLike
Hi Rebecca! Thanks so much for sharing your experiences, they gave me hope for this pregnancy! If you wouldn’t mind, I would love it if you shared the name of the doctor in Pittsburgh who considers breech births with me. I have a slight bicornuate uterus, so regardless of my efforts my baby may stay breech Thanks so much!
Thanks so much!
LikeLike